Fellowship Program
The Interdepartmental Division of Critical Care Medicine (IDCCM) of the University of Toronto currently enjoys a world-wide reputation for Critical Care education and research. Its Royal College training curriculum affords one of the best training programs in Canada and graduates between 8-10 physicians per year, some of whom have remained as faculty.
In addition to the city-wide Royal College Program, there are three hospital-based International Fellowship Programs (University Health Network/Mount Sinai Health, Sunnybrook Health Science Center, and St. Michael’s Hospital) that independently recruit and train approximately 28 fellows per year, accounting for the majority of the clinical fellows in the Division.
It is important to note that the critical care fellowship is not a pathway towards certification and licensure as a Canadian physician. Our program does not provide guidance around application for permanent residency or immigration. Please visit or contact Immigration, Refugees and Citizenship Canada (IRCC) directly for information regarding the immigration process: https://www.canada.ca/en/services/immigration-citizenship.html
The University Health Network and Mount Sinai Hospital Program began in 2001 with the appointment of its first internationally trained medical graduate, Dr. Andrew Jones. Dr. Jones was a Senior Registrar (Senior Fellow) in Medicine from London, UK, with an interest in Critical Care Medicine. Following his year in Toronto, he became a Consultant in Intensive Care at Guy’s and St. Thomas’ Hospital, London and a Senior Lecturer with the University of London.
Under the direction of two former fellows: Dr. Stuart Reynolds (Fellow 2002-2003, Program Director 2004- 2009) and Dr. Andrew Steel (Fellow 2007-2008, Program Director 2009-2016), the International Fellowship Program has since grown considerably. The appointments for the current academic year include over 30 clinical and research fellows. An alternative way in which we measure our success is that since 2001 we have gained alumni from over 20 countries across six continents.
International fellows spend approximately equal time at our three university hospitals: Toronto General Hospital, Toronto Western Hospital, and Mount Sinai Hospital. In addition to affording fellows the highest standard of general adult intensive care training, each is a tertiary referral centre for subspecialty critical care, as detailed below.
Sinai Health System – SHS
Sinai Health System is world-renowned for its Obstetrical Medicine and High-Risk Pregnancy Departments. The Department of Surgery at the University of Toronto also has an international reputation for sarcoma surgery and HIPEC procedures performed at this hospital. Mount Sinai ICU is a 16 bed closed Medical-Surgical Intensive Care Unit that serves not only Mount Sinai but also provides critical care services to the adjacent Princess Margaret Hospital. The Mount Sinai ICU is a primary oncological-focused ICU with a case-mix comprising of patients with hematological malignancies and bone marrow transplantation. The case mix also includes high-risk obstetrical patients, general medical cases, and post-operative surgical oncology.
Areas of clinical expertise and research interest include the ventilator management of ARDS, management of the bone-marrow transplant patient, and critical illness in pregnancy. The ICU provides conventional and non-conventional ventilator support, including high frequency oscillation, and NAVA, and utilizes adjuncts to assess respiratory failure including EIT and esophageal balloon. Dialysis is performed as Continuous Renal Replacement Therapy initiated by the ICU staff and monitored by the Nephrology Unit, as well as intermittent hemodialysis by the Nephrology Unit.
The multidisciplinary team comprises of a full time pharmacist, dietitian, physiotherapist and social worker, in addition to the medical staff and active academic Nursing and Respiratory Therapy departments. The ICU is run on a two intensivist-led model: one attending intensivist is responsible for the MSICU patients, and the second intensivist is responsible for the Rapid Response Team called ACCESS.
Toronto General Hospital – TGH
Toronto General Hospital is a university hospital with 417 beds providing secondary and tertiary care in the heart of Toronto. Toronto General Hospital is acclaimed for its cardio-thoracic and transplant programs. In addition, it is the only centre in Ontario providing extracorporeal life support (ECLS) for respiratory and cardio-pulmonary failure. The multi-organ transplant program is Canada’s largest organ transplant program. More than 500 transplants are performed each year, and more than 5000 recipients are followed by a multidisciplinary team. The hospital also comprises a coronary and cardio-vascular intensive care unit caring for patients with primary cardiac pathologies and post cardiac surgery patients respectively.
Toronto General Hospital has a 24 bed Medical Surgical Intensive Care Unit, which specializes in post transplant care (mainly lung and liver transplant), and respiratory and cardiac failure. Our unit is an ECMO (Extracorporeal Membrane Oxygenation) referral center and 80 patients were placed on ECLS last year, supporting patients with refractory cardio-respiratory failure from the Greater Toronto Area and beyond.
Clinical care coverage is provided by a 2 team-model, each led by a fellow and staff intensivist, with half of the residents allocated to each team. Our CCRT (Critical Care Response Team) also attends to deteriorating patients already admitted in the hospital.
Education is led by fellows and attending physicians with a mixture of didactic lectures and bedside teaching. Our educational program covers general critical care topics, post transplant care, ECLS management, and critical care echocardiography. Fellow-specific teaching focuses on advanced modes of mechanical ventilation, specific aspects of post lung transplant care and ECLS in collaboration with transplant teams and perfusionists. We offer biweekly joint journal club with Toronto Western and Mount Sinai Hospital.
Toronto Western Hospital – TWH
Toronto Western Hospital is located in the vibrant heart of the downtown communities of South Annex, Chinatown, Little Italy, Little Portugal and Queen Street West. It is a 270-bed academic health science centre with a world-leading specialty program in neuroscience, the Krembil Neuroscience Program. The hospital also has a strong community focus, providing emergency care and innovative outpatient programs for its large multicultural surrounding population. With expertise in musculoskeletal health and arthritis, the hospital’s programs also include orthopaedics, rheumatology, ophthalmology, and the hand program. The bariatric comprehensive program offers medical and surgical care for candidates for bariatric surgery. Finally, its busy Emergency Department sees more than 60,000 patients annually.
Toronto Western Hospital has a 25-bed Medical-Surgical and Neuroscience Intensive Care Unit. The TWH MSNICU admits approximately 950 medical-surgical and brain-injured patients per year, with a case mix of 55-60% general critical care patients and 40-45% neuroscience patients (acute ischemic stroke, subarachnoid hemorrhage, intracranial hemorrhage, traumatic brain injury, spinal cord injury, and neuromuscular disease). The ICU has a busy Critical Care Response Team, handling more than 900 emergency consults per year.
Clinical coverage is provided with a two-team model. Each team is comprised of an intensivist, a designated fellow, and half of the resident house staff. The Critical Care Response Team includes one of the two intensivists, a fellow and a critical care nurse.
Education at the Toronto Western Hospital ICU is delivered by attending physicians, fellows, and the multidisciplinary team. Education focuses on general critical care topics, with a special focus on neurocritical care. Each week of the rotation focuses on different aspects of critical care (e.g., principles of acute resuscitation and shock management, neurocritical care, respiratory failure and principles of mechanical ventilation, toxicology, best practices in ICU). Fellow-specific education includes weekly fellow seminars and bimonthly journal club. Other valuable learning opportunities for both residents and fellows include neuroscience rounds (EEG, neuroimaging), monthly M&M rounds, and bimonthly journal club sessions.
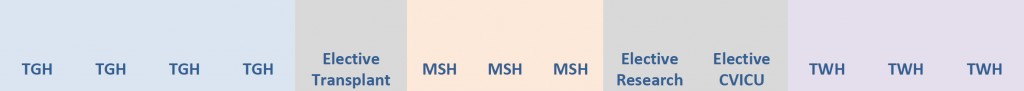
UHN/MSH General Critical Care Program – example rotation schedule:
Each rotation period is 4 weeks long, with fellows spending not less than 12 weeks at each site. This enables fellows to completely integrate into the ICU team and develop their clinical knowledge and leadership skills that come with the familiarity of the workplace and its local practices.
Subspecialty Fellowships (for second year or equivalent only)
Second (or higher) year UHN/Sinai fellows may be eligible to apply for subspecialty programs, such as hemato-oncologic critical care, neurocritical care, ECLS, or critical care echocardiography.
Please contact us for more information.
Fellows are also able to broaden their experience through periods of up to 8 weeks of elective training in complementary disciplines. Fellows who express an interest in specific areas can have their rotation specifically planned to accommodate their educational objectives. This enables fellows to cultivate a niche within the specialty which is vital for career advancement, research development, and strengthening the overall appeal of the program to senior trainees. From the perspective of the department, fellows undertaking external electives serve as our ambassadors and facilitate broader collaboration with our colleagues in the Faculty of Medicine. Electives have been arranged in specialties such as:
Core Subspecialty ICU Training
- Airway Management Techniques
- Transport of the Critically ill
- Solid Organ Transplant
- Extracorporeal Life Support
- Pediatric ICU
- Anesthesia
- Infectious Diseases
- Cardiovascular ICU
- Continuity of Care
- Emergency Medicine
- Trauma and Burns
- Cardiopulmonary Exercise Testing
Subspecialty Fellowships (for second year or equivalent only)
Second (or higher) year fellows may be eligible to apply for subspecialty programs such as hemato-oncologic critical care, neuro critical care, ECLS, or critical care echocardiography.
Fellows who have completed at least 12 months of clinical critical care in a Royal College accredited program or equivalent may also be eligible. Conditions will apply. Please contact us for more information.
Subspecialty Examination Affiliate Program (SEAP)
*Please note that SEAP is not currently available (updated April 2024)
In March 2014, the Royal College of Physicians and Surgeons of Canada Council approved a proposal to create an examination program and affiliate category for non-certified subspecialists. To be eligible for the examination in Critical Care Medicine, fellows would have to meet Royal College requirements and this will include successful completion of a two-year training program that is, to all intents and purposes, identical to that of the Royal College Residency.
SEAP does not create a new pathway to Royal College Fellowship, nor can successful subspecialty exam candidates use the FRCPC or FRCSC designation. The Affiliate status provides a mechanism for maintaining engagement with the Royal College and participating in the Maintenance of Certification (MOC) Program. It does not confer Royal College membership or Fellowship status; however, those who pass the exam will be provided a Royal College attestation of their successful completion and offered the option to become a Royal College Subspecialist Affiliate.
If this examination pathway is of interest to you and of value to your future career in Critical Care Medicine, then it is important to complete a specific Clinical Fellowship Program that will meet College requirements. This will need to be confirmed with the Program Director’s office before commencement.
All fellows are enrolled as full-time postgraduate students; the program is affiliated with the University of Toronto, Temerty Faculty of Medicine, and upon successful completion, our fellows are awarded certificates from both the University and the Interdepartmental Division of Critical Care Medicine. Fellows are actively encouraged to pursue higher qualifications and many choose to sit the American Board of Internal Medicine Critical Care and the European Diploma of Intensive Care examinations.
The well-structured and comprehensive teaching provided through our program has proved invaluable to those preparing for examinations. Protected time for research and the pursuit of academic goals is available, and the clinical fellows will participate in and present at aspects of the following academic schedule:
Education Sessions
- Daily, critical care teaching delivered by attending staff at each hospital site
- Weekly, Academic ½ Day Critical Care City-‐Wide Fellows Rounds delivered by attending staff from Critical Care and associated specialties
- Weekly, site-specific Hospital Grand Rounds
- Weekly, site-specific Critical Care Inter-professional Rounds
- Weekly, site-specific Antimicrobial Stewardship Rounds
- Weekly, ECLS rounds (Toronto General Hospital)
- Monthly, university division Clinical Research in Progress Rounds
- Monthly, University Health Network Clinical Research Rounds
- Monthly, site-specific Critical Care Morbidity and Mortality Meeting
- Annual Critical Care Canada Fellows Day, part of the Critical Care Canada Forum in Toronto
As a centre for both clinical and academic excellence, the Interdepartmental Division of Critical Care Medicine provides ample opportunities for those with research interests. Benefiting from the experience and mentorship of global leaders in critical care research, fellows are able to refine their academic writing and critical appraisal skills and develop and conduct practical projects. The regular Clinical Research in Progress rounds and journal clubs are essentially research master classes where ideas, methodologies and critical appraisal skills are developed and refined. There are numerous academic meetings that are held within the Faculty of Medicine which attract local, national, and international experts. They provide invaluable opportunities to develop academic knowledge and research skills, and compliment the divisional program.
It is a credit to both fellows and faculty that almost all of our fellows complete and publish (authored or co-‐authored) an original article, systematic review, or editorial. In addition, more than 70% of fellows publish and present in abstract at either national or international congresses.
It is important to note that the opportunity to participate in research during the fellowship is very good, but could be improved. We afford protected time for research and our fellows really value this. By further encouraging that work produced on behalf of the University is presented at either a national or international congress, we provide an excellent training opportunity and vital global impact for the division.
Individuals who are interested in pursuing a research career and further experience in clinical, basic, and educational research are encouraged to meet early on with our research director Dr. Eddy Fan (UHN) and research leads, Dr. Michael Detsky (MSH), Dr. Lorenzo Del Sorbo (TGH), and Dr. Elizabeth Wilcox (TWH) . Many opportunities exist across the University and affiliated institutions, and the large number of faculty is central to the success of our research programs. The number of departments, faculty, and their diversity of interests allow fellows the opportunity to develop their research interests in a collaborative environment.